- South Texas Students Meet Accordion Music Icons Los Tigres Del Norte In Edinburg Thanks To Khs America/Hohner Alianza Académica Initiative
- Fragile Planet Offers a Nighttime Wildlife Experience
- Falcons Soccer Off & Running
- Cameron County Receives Funds to Improve Two Parks
- Falcons Complete First Half of 32-6A
- School District to Help out Victims of California Wildfires
- Sand Castle Days Continued Despite Unexpected Weather
- Ready for District
- Discussion of Garbage Dumpster Rates, Agreements Between State & City on Highway Regulations, and More
- 31st Annual Shrimp Cook-Off is Right Around the Corner
Alzheimer’s Study Links Cholesterol And Toxic Protein Clusters
- Updated: March 10, 2023
Department of Biochemistry and Biophysics study more closely connects diet and Alzheimer’s disease development
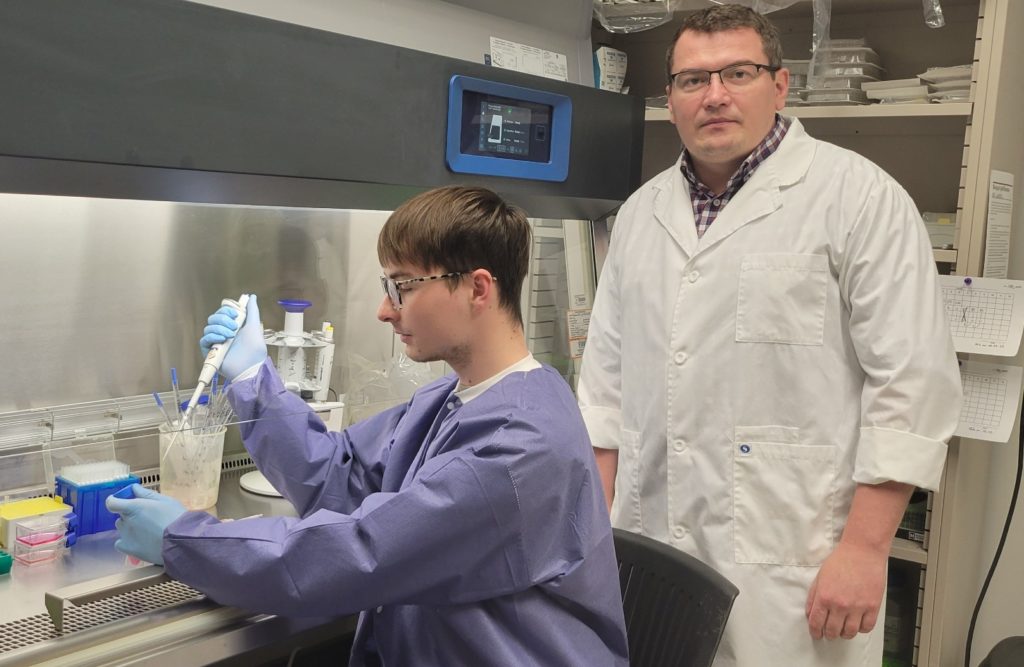
Written by Paul Schattenberg
Cholesterol tremendously increases the toxicity of a peptide implicated in Alzheimer’s progression, according to research by scientists in the Department of Biochemistry and Biophysics in Texas A&M’s College of Agriculture and Life Sciences.
The study, “Lipids uniquely alter the secondary structure and toxicity of amyloid beta 1-42 aggregates,” by Dmitry Kurouski, Ph.D., and research assistants Kiryl Zhaliazka and Mikhail Matyeyenka, was supported by a $1.5 million Maximizing Investigators’ Research Award from the National Institutes of Health. It was published in FEBS Journal — the journal of the Federation of European Biochemical Societies.
“The study found that certain lipids can increase the toxicity of amyloid beta peptides, which are thought to play a role in the development of Alzheimer’s disease,” said Kurouski, an assistant professor and primary investigator for the study, Bryan-College Station. “Specifically, we discovered that the interaction between amyloid beta and lipids can cause the formation of small, toxic clusters called oligomers.”
Additionally, the study showed these lipids can alter the basic shape, or the secondary structure, of amyloid beta peptides, which can further increase their toxicity.
“This provides new insights into the mechanisms behind the toxic effects of amyloid beta in the brain,” Kurouski said.
He said the results of the study show a strong connection between Alzheimer’s disease and the change in the lipid composition of neuronal membranes, which, in turn, can be affected by a person’s diet.
About Alzheimer’s disease
Alzheimer’s disease causes the brain to shrink and brain cells to eventually die. It is the most common cause of dementia — a gradual decline in memory, thinking, behavior and social skills — affecting a person’s overall ability to function.
Alzheimer’s is characterized by protein fragments called amyloid beta, which deposit in the spaces between nerve cells. These protein fragments can clump together to form amyloid plaques thought to be a factor in the onset of senility.
“While the precise mechanisms underlying Alzheimer’s disease are not fully understood, there is evidence to suggest that the buildup of amyloid beta peptides in the brain plays a role in the development of the disease,” Kurouski said. “Specifically, it is thought that the aggregation of amyloid beta into plaques can disrupt communication between neurons and ultimately lead to cell death.”
He said the relationship between amyloid beta plaques and Alzheimer’s disease is complex, and other factors such as inflammation and the accumulation of another protein called tau are also thought to be involved.
“Amyloid peptides, including amyloid beta, are known to interact with lipids in the brain,” Kurouski said. “These interactions can play a role in the formation of amyloid plaques and the pathology of Alzheimer’s disease.”
While not all amyloid peptides necessarily interact with lipids in the brain, the study found the oligomers formed in the presence of lipids were more toxic than other forms of amyloid beta.
“This suggests the interaction may be particularly important in regard to the harmful effects of amyloid beta in Alzheimer’s disease,” he said.
Study results
The study showed three different lipids — phosphatidylcholine, cardiolipin and cholesterol — strongly accelerated the rate of fibril formation compared to the rate of amyloid beta aggregation when no lipids were present. It also showed that cardiolipin allowed for the strongest acceleration of amyloid beta aggregation.
Futhermore, phosphatidylcholine, cardiolipin and cholesterol each uniquely altered the secondary structure of early, middle- and late-stage amyloid beta aggregates, Kurouski said.
“Specifically, cardiolipin and cholesterol drastically increased the amount of amyloid beta oligomers and fibrils grown in the presence of these lipids,” he said. “This caused a significant increase in the toxicity when compared to the toxicity of aggregates formed in a lipid-free environment.”
Dietary implications
Kurouski said the results allowed them to conclude that the secondary structure of amyloid beta fibrils directly depends on the lipid present in the protein solution upon their formation.
He also said there is evidence to suggest that dietary factors may influence the lipid composition of neuronal membranes.
“In the convergence of nutrition and human health, a diet that limits the amount of cholesterol, especially low-density lipoprotein cholesterol, and phospholipids can be important in reducing the ability of these lipids to react with the amyloid beta peptides,” he said.
Kurouski said research has shown that certain dietary fats, such as omega-3 fatty acids, have been shown to be important for maintaining the integrity and function of neuronal membranes.
“Additionally, studies have shown that dietary interventions, such as calorie restriction, can alter the lipid composition of neuronal membranes in animal models.”
He said study results may also support the idea that therapeutics be directed not on the amyloid beta peptide itself, as has been done to date, but more specifically on the interactions between lipids and amyloid beta peptides.
“Such interactions lead to the formation of highly toxic protein-lipid complexes that are far more toxic than amyloid beta oligomers themselves,” he said.
Study limitations
Kurouski said one limitation of the study is that it was conducted in cell-based assays rather than in living organisms, so it is not clear how the findings will translate to the complex environment of the brain. Additionally, the research only investigated a limited number of lipids, so it is possible that other types of lipids may also play a role in the harmful effects of amyloid beta.
“The next step of the study is to further investigate the underlying molecular mechanisms of the interaction between amyloid beta peptides and lipids,” Kurouski said.
He said that demonstrating the connection between toxicity and Alzheimer’s disease progression would require extensive testing on humans. However, before such studies can be conducted, preclinical studies in animal models would need to be performed to establish the safety and efficacy of any potential therapeutic interventions.
“It is important to note that while this study provides valuable insights into the role of lipid interaction in amyloid beta toxicity, additional research is needed before any clinical applications can be developed,” Kurouski said.